The Impact of Patient–Physician Racial and Gender Concordance on Patient Satisfaction with Outpatient Clinic Visits

Patient and provider race and gender concordance (patient and physician identify as the same race/ethnicity or gender) may impact patient experience and satisfaction.
Objective
We sought to examine how patient and physician racial and gender concordance effect patient satisfaction with outpatient clinical encounters. Furthermore, we examined factors that changed satisfaction among concordant and discordant dyads.
Design
Consumer Assessment of Healthcare Provider and Systems (CAHPS) Patient Satisfaction Survey Scores were collected from outpatient clinical encounters between January 2017 and January 2019 at the University of California, San Francisco.
Participants
Patients who were seen in the eligible time period, who voluntarily provided physician satisfaction scores. Providers with fewer than 30 reviews and encounters with missing data were excluded.
Main Measures
Primary outcome was rate of top satisfaction score. The provider score (1–10 scale) was dichotomized as “top score (9-10)” and “low scores (<9).”
Key Results
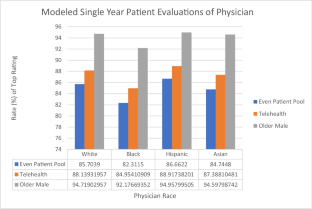
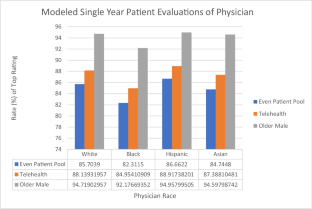
A total of 77,543 evaluations met inclusion criteria. Most patients identified as White (73.5%) and female (55.4%) with a median age of 60 (IQR 45, 70). Compared to White patients, Asian patients were less likely to give a top score even when controlling for racial concordance (OR: 0.67; CI 0.63–0.714). Telehealth was associated with increased odds of a top score relative to in-person visits (OR 1.25; CI 1.07–1.48). The odds of a top score decreased by 11% in racially discordant dyads.
Conclusions
Racial concordance, particularly among older, White, male patients, is a nonmodifiable predictor of patient satisfaction. Physicians of color are at a disadvantage, as they receive lower patient satisfaction scores, even in race concordant pairs, with Asian physicians seeing Asian patients receiving the lowest scores. Patient satisfaction data is likely an inappropriate means of determining physician incentives as such may perpetuate racial and gender disadvantages.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save
Springer+ Basic
€32.70 /Month
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Buy Now
Price includes VAT (France)
Instant access to the full article PDF.
Rent this article via DeepDyve

Similar content being viewed by others

The Association Between Physician Race/Ethnicity and Patient Satisfaction: an Exploration in Direct to Consumer Telemedicine
Article 06 July 2020
The association between Asian patient race/ethnicity and lower satisfaction scores
Article Open access 22 July 2020

Differential Effect of Patient- and Provider-Level Factors on Patient Satisfaction Scores in Academic General Internal Medicine Clinics
Article 01 February 2024
Explore related subjects
Data Availability
Data will not be made available.
Code Availability
Code can be made available without associated data.
References
- Olaisen RH, Schluchter MD, Flocke SA, Smyth KA, Koroukian SM, Stange KC. Assessing the longitudinal impact of physician-patient relationship on functional health. Ann Fam Med. 2020;18(5):422–9. https://doi.org/10.1370/AFM.2554. ArticlePubMedPubMed CentralGoogle Scholar
- Martinez KA, Keenan K, Rastogi R, et al. The association between physician race/ethnicity and patient satisfaction: an exploration in direct to consumer telemedicine. J Gen Intern Med. 2020;35(9):2600–6. https://doi.org/10.1007/S11606-020-06005-8. ArticlePubMedPubMed CentralGoogle Scholar
- Takeshita J, Wang S, Loren AW, et al. Association of racial/ethnic and gender concordance between patients and physicians with patient experience ratings. JAMA Netw Open. 2020;3(11):e2024583. https://doi.org/10.1001/jamanetworkopen.2020.24583. ArticlePubMedPubMed CentralGoogle Scholar
- Jackson JL, Chamberlin J, Kroenke K. Predictors of patient satisfaction. Soc Sci Med. 2001;52(4):609–20. https://doi.org/10.1016/S0277-9536(00)00164-7. ArticleCASPubMedGoogle Scholar
- Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282(6):583–9. https://doi.org/10.1001/JAMA.282.6.583. ArticleCASPubMedGoogle Scholar
- Murphy GP, Awad MA, Tresh A, et al. Association of patient volume with online ratings of California urologists. JAMA Surg. 2018;153(7):685–6. https://doi.org/10.1001/JAMASURG.2018.0149. ArticlePubMedPubMed CentralGoogle Scholar
- Murphy GP, Radadia KD, Breyer BN. Online physician reviews: is there a place for them? Risk Manag Healthc Policy. 2019;12:85–9. https://doi.org/10.2147/RMHP.S170381. ArticlePubMedPubMed CentralGoogle Scholar
- Murphy GP, Awad MA, Osterberg EC, et al. Web-based physician ratings for California physicians on probation. J Med Internet Res. 2017;19(8). https://doi.org/10.2196/JMIR.7488.
- Petrullo KA, Lamar S, Nwankwo-Otti O, Alexander-Mills K, Viola D. The patient satisfaction survey: what does it mean to your bottom line? J Hosp Adm. 2013;2(2). https://doi.org/10.5430/jha.v2n2p1.
- Siegrist RB. Patient satisfaction: history, myths, and misperceptions. Virtual Mentor. 2013;15(11):982–7. https://doi.org/10.1001/VIRTUALMENTOR.2013.15.11.MHST1-1311. ArticlePubMedGoogle Scholar
- Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Arch Intern Med. 1999;159(9):997–1004. https://doi.org/10.1001/ARCHINTE.159.9.997. ArticleCASPubMedGoogle Scholar
- Haviland MG, Morales LS, Reise SP, Hays RD. Do health care ratings differ by race or ethnicity? Jt Comm J Qual Saf. 2003;29(3):134–45. https://doi.org/10.1016/s1549-3741(03)29016-x. ArticlePubMedGoogle Scholar
- Murray-García JL, Selby JV, Schmittdiel J, Grumbach K, Quesenberry CPJ. Racial and ethnic differences in a patient survey: patients’ values, ratings, and reports regarding physician primary care performance in a large health maintenance organization. Med Care. 2000;38(3):300–10. https://doi.org/10.1097/00005650-200003000-00007. ArticlePubMedGoogle Scholar
- Kumar D, Schlundt DG, Wallston KA. Patient-physician race concordance and its relationship to perceived health outcomes. Ethn Dis. 2009;19(3):345–51. PubMedGoogle Scholar
- LaVeist TA, Nuru-Jeter A, Jones KE. The association of doctor-patient race concordance with health services utilization. J Public Health Policy. 2003;24(3-4):312–23. https://doi.org/10.2307/3343378. ArticlePubMedGoogle Scholar
- Laveist TA, Nuru-Jeter A. Is doctor-patient race concordance associated with greater satisfaction with care? J Health Soc Behav. 2002;43(3):296–306. ArticlePubMedGoogle Scholar
- Taira DA, Safran DG, Seto TB, et al. Do patient assessments of primary care differ by patient ethnicity? Health Serv Res. 2001;36(6 Pt 1):1059–71. CASPubMedPubMed CentralGoogle Scholar
- Wallis CJD, Jerath A, Coburn N, et al. Association of surgeon-patient sex concordance with postoperative outcomes. JAMA Surg. 2021. https://doi.org/10.1001/JAMASURG.2021.6339.
- Meghani SH, Brooks JM, Gipson-Jones T, Waite R, Whitfield-Harris L, Deatrick JA. Patient-provider race-concordance: does it matter in improving minority patients’ health outcomes? Ethn Health. 2009;14(1):107–30. https://doi.org/10.1080/13557850802227031. ArticlePubMedPubMed CentralGoogle Scholar
- Rogo-Gupta LJ, Haunschild C, Altamirano J, Maldonado YA, Fassiotto M. Physician gender is associated with Press Ganey patient satisfaction scores in outpatient gynecology. Women’s Heal issues Off Publ Jacobs Inst Women’s Heal. 2018;28(3):281–5. https://doi.org/10.1016/j.whi.2018.01.001. ArticleGoogle Scholar
- Woods SE, Heidari Z. The influence of gender on patient satisfaction. J gender-specific Med JGSM Off J Partnersh Women’s Heal Columbia. 2003;6(4):30–5. Google Scholar
- Okunrintemi V, Valero-Elizondo J, Patrick B, et al. Gender differences in patient-reported outcomes among adults with atherosclerotic cardiovascular disease. J Am Heart Assoc. 2018;7(24):e010498. https://doi.org/10.1161/JAHA.118.010498. ArticlePubMedPubMed CentralGoogle Scholar
- Alsaif A, Alqahtani S, Alanazi F, Alrashed F, Almutairi A. Patient satisfaction and experience with anesthesia: a multicenter survey in Saudi population. Saudi J Anaesth. 2018;12(2):304–10. https://doi.org/10.4103/sja.SJA_656_17. ArticlePubMedPubMed CentralGoogle Scholar
- U.S. Census Bureau QuickFacts: San Francisco County, California. https://www.census.gov/quickfacts/fact/table/sanfranciscocountycalifornia/POP010220. Accessed November 14, 2022.
- Patel I, Chang J, Srivastava J, Feldman S, Levender M, Balkrishnan R. Patient satisfaction with obstetricians and gynecologists compared with other specialties: analysis of US self-reported survey data. Patient Relat Outcome Meas. 2011;2:21–6. https://doi.org/10.2147/PROM.S15747. ArticlePubMedPubMed CentralGoogle Scholar
- Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8):e016242. https://doi.org/10.1136/BMJOPEN-2017-016242. ArticlePubMedPubMed CentralGoogle Scholar
- Ramaswamy A, Yu M, Drangsholt S, et al. Patient satisfaction with telemedicine during the COVID-19 pandemic: retrospective cohort study. J Med Internet Res. 2020;22(9):e20786. https://doi.org/10.2196/20786.
- Mueller BR, Lawrence S, Benn E, et al. Disparities in telehealth utilization in patients with pain during COVID-19. Pain Reports. 2022;7(3):E1001. https://doi.org/10.1097/PR9.0000000000001001. ArticlePubMedPubMed CentralGoogle Scholar
- Campos-Castillo C, Anthony D. Racial and ethnic differences in self-reported telehealth use during the COVID-19 pandemic: a secondary analysis of a US survey of internet users from late March. J Am Med Inform Assoc. 2021;28(1):119. https://doi.org/10.1093/JAMIA/OCAA221. ArticlePubMedGoogle Scholar
- Brown SH, Griffith ML, Kripalani S, Horst SN. Association of health literacy and area deprivation with initiation and completion of telehealth visits in adult medicine clinics across a large health care system. JAMA Netw Open. 2022;5(7):e2223571–1. https://doi.org/10.1001/JAMANETWORKOPEN.2022.23571. ArticlePubMedPubMed CentralGoogle Scholar
- Chang ES, Simon M, Dong XQ. Integrating cultural humility into health care professional education and training. Adv Health Sci Educ Theory Pract. 2012;17(2):269–78. https://doi.org/10.1007/S10459-010-9264-1. ArticlePubMedGoogle Scholar
- Tang C, Tian B, Zhang X, et al. The influence of cultural competence of nurses on patient satisfaction and the mediating effect of patient trust. J Adv Nurs. 2019;75(4):749–59. https://doi.org/10.1111/JAN.13854. ArticlePubMedGoogle Scholar
- Davidson KW, Shaffer J, Ye S, et al. Interventions to improve hospital patient satisfaction with healthcare providers and systems: A systematic review. BMJ Qual Saf. 2017;26(7):596. https://doi.org/10.1136/BMJQS-2015-004758. ArticlePubMedGoogle Scholar
- Argueza BR, Saenz SR, McBride D. From diversity and inclusion to antiracism in medical training institutions. Acad Med. 2021;96(6):798–801. https://doi.org/10.1097/ACM.0000000000004017. ArticlePubMedPubMed CentralGoogle Scholar
- Liao L, Chung S, Altamirano J, et al. The association between Asian patient race/ethnicity and lower satisfaction scores. BMC Health Serv Res. 2020;20(1):678. https://doi.org/10.1186/s12913-020-05534-6. ArticlePubMedPubMed CentralGoogle Scholar
- Butler C, Baskin AS, Mmonu NA, et al. Patient satisfaction in a safety net urology clinic. Urol Pract. 2021;8(2):168–75. https://doi.org/10.1097/UPJ.0000000000000177. ArticlePubMedGoogle Scholar
- Saha S, Hickam DH. Explaining low ratings of patient satisfaction among Asian-Americans. Am J Med Qual Off J Am Coll Med Qual. 2003;18(6):256–64. https://doi.org/10.1177/106286060301800606. ArticleGoogle Scholar
- Alfred M, Ubogaya K, Chen X, Wint D, Worral PS. Effectiveness of culturally focused interventions in increasing the satisfaction of hospitalized Asian patients: a systematic review. JBI Database Syst Rev Implement Reports. 2016;14(8):219–56. https://doi.org/10.11124/JBISRIR-2016-003048. ArticleGoogle Scholar
- Truong M, Paradies Y, Priest N. Interventions to improve cultural competency in healthcare: a systematic review of reviews. BMC Health Serv Res. 2014;14(1):1–17. https://doi.org/10.1186/1472-6963-14-99/TABLES/1. ArticleGoogle Scholar
- Dunsch F, Evans DK, Macis M, Wang Q. Bias in patient satisfaction surveys: a threat to measuring healthcare quality. BMJ Glob Heal. 2018;3(2):694. https://doi.org/10.1136/BMJGH-2017-000694. ArticleGoogle Scholar
Acknowledgements
We gratefully acknowledge the assistance of Nizar Hakam, Behnam Nabavizadeh, Natalie Rios, and Michael Sadighian particularly for their roles in reviewing provider profiles. All represent the UCSF Department of Urology and were otherwise uncompensated for their work.
Author information
- Diane Sliwka and Benjamin N. Breyer contributed equally to this work.
Authors and Affiliations
- Department of Urology, University of California San Francisco, San Francisco, CA, USA Nathan M. Shaw, Jordan Holler & Benjamin N. Breyer
- Department of Urology, MedStar Georgetown University Hospital, Washington, DC, USA Nathan M. Shaw
- Department of Epidemiology and Biostatistics, University of California San Francisco, 1001 Potrero Suite 3A, San Francisco, CA, 94110, USA Nancy Hills & Benjamin N. Breyer
- Department of Neurology, University of California San Francisco, San Francisco, CA, USA Nancy Hills
- Harvard T.H. Chan School of Public Health, Boston, MA, USA Jordan Holler
- Department of Medicine, University of California San Francisco, San Francisco, CA, USA Alicia Fernandez, Denise Davis, Nynikka R. Palmer & Diane Sliwka
- Division on General Internal Medicine at Zuckerberg San Francisco General Hospital, University of California San Francisco, San Francisco, CA, USA Alicia Fernandez & Nynikka R. Palmer
- Nathan M. Shaw